Translational Science Benefits
Summary
This project involved two aligned laboratory discoveries. First, Duke’s scientists were able to significantly soften human fibroid tissue by injecting a highly purified enzyme that can degrade the collagen in fibroids (Clostridium Histolyticum collagenase [CHC]). Second, North Carolina Central University scientists pioneered the development of a breakthrough injectable hydrogel-copolymer (LiquoGelTM) that allows delivery of a high drug payload; this can be a single drug or a cocktail drug mixture, and it can include and deliver water-soluble and non-water-soluble drugs. These two discoveries permitted novel testing of injectable drug delivery to evaluate treatment for uterine fibroids by local injections.
To conduct this research, chemists at North Carolina Central University developed standard operating procedures for the preparation of larger batches (20 g) of LiquoGelTM with purity in excess of 98% as confirmed by nuclear magnetic resonance spectroscopy. The LiquoGelTM carrier is liquid at room temperature and transitions to a gel at normal body temperatures. This protects locally delivered therapeutic drugs. Such drugs and other substances can be “entrapped” in the “pores” of the hydrogel copolymer. The team was also able to develop batches of LiquoGelTM with more firmly (covalently) bound substances (LiquoGelTM– R) that can also be loaded with other drugs. More firmly bound substances could be used as markers, or “beacons”, for treatment or diagnostic applications.
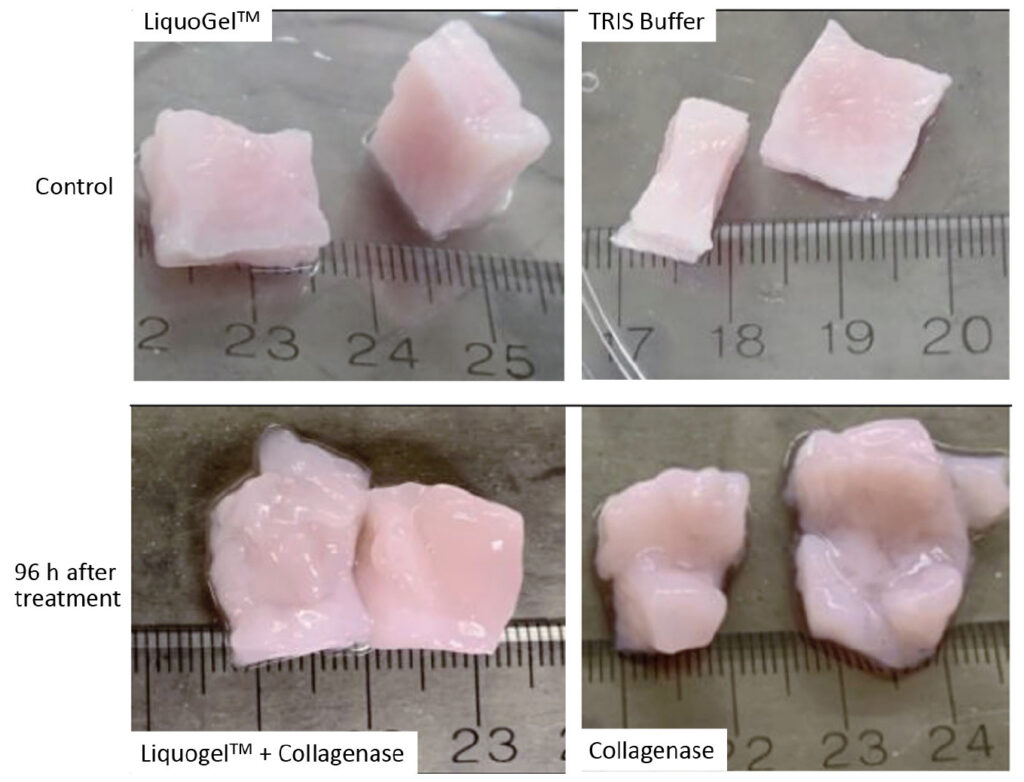
Working with Duke clinicians and scientists, human uterine fibroid tissue was then collected after routine surgery. In the laboratory, the team evaluated the degradation/softening of these fibroid tissues at various time points after injection with CHC with and without LiquoGelTM. To characterize and quantify the effects of local CHC injections on collagen, the microscopic structure of these tissues was examined and the stiffness modulus and viscoelasticity of the uterine fibroid tissues were measured. Injected fibroid tissues were ultimately liquefied or exhibited gel-like behavior.
The results of this intervention show promise for the development of injectable and localized enzymatic therapies for uterine fibroids and other dense tumors. In this pilot study, CHC injections reduced the tissue modulus by over two orders of magnitude, and co-injection of LiquoGelTM enhanced this effect. This unprecedented approach to delivering drugs locally via LiquoGelTM can avoid systemic side effects and treat uterine fibroid tumors. Leveraging this targeted technology could transform uterine fibroid therapy by offering a minimally invasive and non-surgical injectable alternative treatment that allows patients to keep their uterus thus reducing morbidity and costs associated with this disease.
Initial cytotoxicity studies have been done ex-vivo and in mice, but injection of the drug delivery polymer into a human cavity has to undergo in-vivo trials. Through a recently awarded NC Biotechnology TRG grant, the team is currently fine-tuning the parameters needed to scale up production of the polymer and to further test the added benefit of drug delivery in combination with LiquoGelTM.
Significance
Uterine fibroids are common reproductive-age tumors. More than 80% of Black women and nearly 70% of White women have fibroids by age 50. Uterine fibroids are stiff tumors that contain a significant amount of collagen and can become quite large. While they are non-cancerous, they can contribute to severe morbidity (pain, bleeding, anemia) and infertility. Fibroids are the leading cause of hysterectomies in the U.S. Yet, many women want to keep their uterus. Existing minimally invasive surgical procedures that preserve the uterus are expensive and are performed only at major medical centers. Reinterventions are commonly required (up to 50%) to treat regrown or new fibroids. Currently available drug therapies have significant systemic side effects. The personal and medical management of these benign tumors costs tens of billions annually in the U.S.—more than twice the cost of breast cancer.
Workforce development & diversity
Darlene Taylor was an NIH K12 BIRCWH Scholar (06/01/2008–05/31/2013). These five years of BIRCWH support facilitated engagement in a suite of biological topics (i.e., five Clinical Research Training Program courses, Molecular Biology Workshop 2009, uterine fibroids, breast cancer tumors, etc.). Together, her unique biological/polymer physical training positioned Dr. Taylor to attract external funding ($471k), deliver eight (8) presentations, and publish her research in peer-reviewed journals. She was also able to: 1) launch a quality polymer biomaterials initiative at NC Central that focuses on addressing women’s health through advanced polymer materials; 2) obtain promotion and tenure to associate professor and receive the adjunct appointment at Duke and in BRITE (a research-intensive program at NC Central); and 3) pioneer the development of a novel drug delivery platform, namely LiquoGelTM. Now as a full professor in the Department of Chemistry and Biochemistry at NCCU, Dr. Taylor has built a network of research collaborators to pursue innovative delivery options of therapeutic agents for tumors affecting the health of women.
Health equity & disparities
Black women have a greater disease burden and a hysterectomy rate for fibroids three-fold higher than White women. Black women develop uterine fibroids at an earlier age resulting in a greater need to utilize uterus-preserving treatment modalities. A new minimally invasive treatment of fibroids would especially benefit these women who want to preserve their uterus. Local delivery under ultrasound guidance using IVF needles is feasible. Our results show promise for the development of injectable and localized enzymatic therapies for uterine fibroids and other dense tumors.
Benefits
Demonstrated benefits are those that have been observed and are verifiable.
Potential benefits are those logically expected with moderate to high confidence.
Refinement of an ex-vivo model for testing enzymatic degradation of extracellular matrix in human fibroids using injections, incubation, histology, and rheology. demonstrated.
Clinical
Development, testing, and refinement of a drug delivery system that can be used in uterus-preserving, minimally invasive therapy for the treatment of uterine fibroids (or other dense tumors). Collagen degrading enzymes or other drugs can be targeted to work locally, thereby reducing or eliminating drug systemic side effects. potential.
Clinical
Development, testing, and refinement of a drug delivery system that can be used in local drug delivery. The delivery system entraps or covalently binds a wide range of drug classes. It is liquid at room temperature and transitions to a gel at body temperature. potential.
Clinical
Drug delivery system that can be used in local drug delivery. The delivery system can entrap or covalently bind a high payload and a wide range of drug classes. It is liquid at room temperature and transitions to a gel at body temperature thereby reducing washout and localizing the drug to the place of injection. demonstrated.
Clinical
The uterus-preserving, local injection of fibroids could be performed under ultrasound guidance in a doctor’s office. Women could preserve their uterus and avoid the risk of surgical removal of their uterus and/or fibroids, as well as a hospital stay and long recovery. Since Black women usually develop fibroids earlier during their reproductive life, this patient population would especially benefit from such treatment option. potential.
Community
The availability of a new treatment option that is minimally invasive can decrease barriers for women to seek treatment at an earlier stage in their disease. potential.
Community
The developed and tested drug delivery platform can be licensed for use in fibroids and other diseases that would benefit from local drug delivery. potential.
Economic
Uterine fibroids result in high healthcare costs and loss of productivity in affected women. The management of uterine fibroids is estimated at $34 billion annually in the U.S. Minimally invasive, local treatment of fibroids can offer a more acceptable, less costly, and faster treatment option, thus decreasing women’s suffering and increasing their ability to live a productive life. potential.
Economic
This research has clinical, community, economic, and policy implications. The framework for these implications was derived from the Translational Science Benefits Model created by the Institute of Clinical & Translational Sciences at Washington University in St. Louis.
Clinical
This project resulted in the development, testing, and refinement of a drug delivery system that can be used in uterus-preserving, minimally invasive therapy for the treatment of uterine fibroids (or other dense tumors). The delivery system can entrap or covalently bind a high payload and a wide range of drug classes. It is liquid at room temperature and transitions to a gel at body temperature thereby reducing washout and localizing the drug to the place of injection. Collagen-degrading enzymes or other drugs can be targeted to work locally, thereby reducing or eliminating drug systemic side effects.
Community
Fibroid treatment options are very limited, especially for women with fibroids who want to still have children and for women at high risk for surgical complications. Many women experience high morbidity (i.e. pain, bleeding, anemia, infertility) leading to reduced quality of life and decreased productivity. Society often allows women to suffer in silence and accept gynecologic pain as “normal.” Ultimately, the uterus preserving, local injection of fibroids could be performed under ultrasound guidance in a doctor’s office. Women would not have to take the risk of surgical removal of their uterus and/or fibroids, avoid the hospital stay and long recovery, and preserve their uterus. The availability of a new treatment option that is minimally invasive can decrease barriers for women to seek treatment at an earlier stage in their disease.
Economic
Uterine fibroids result in high healthcare costs and loss of productivity in affected women. The management of uterine fibroids is estimated at $34 billion annually in the U.S. Minimally invasive, local treatment of fibroids can offer a more acceptable, less costly, and faster treatment option, thus decreasing women’s suffering and increasing their ability to live a productive life. The developed and tested drug delivery platform can be licensed for use in fibroids and other diseases that would benefit from local drug delivery.
- Corder RD, Gadi SV, Vachieri RB, et al. Using rheology to quantify the effects of localized collagenase treatments on uterine fibroid digestion. Acta Biomaterialia. 2021;134:443-452.

