Translational Science Benefits
Summary
Invasive fungal sinusitis is a rare but deadly diagnosis. While only about fifteen cases per year occur at any single institution, fifty to eighty percent of cases result in death. People with weakened immune systems, such as those with poorly controlled diabetes, undergoing chemotherapy, or taking chronic immunosuppressive medication, have a higher risk of developing invasive fungal sinusitis. Though only a small percentage of immunocompromised individuals ultimately develop the condition.
Non-invasive fungal sinusitis, also called allergic fungal sinusitis or fungal ball, is the most common form of fungal sinusitis. Though it is considered a benign diagnosis, recent research indicates that fungal sinusitis may be a spectrum of disease, meaning that non-invasive forms of the condition could progress to become invasive. This potential progression is highly concerning, as non-invasive fungal sinusitis is already relatively common and could become more prevalent as exposure to fungus in the environment increases with the rise of extreme climate events. The potential for disease progression is especially concerning for vulnerable immunocompromised groups.
Understanding how invasive fungal sinusitis develops in the body and the specific factors that make some individuals more susceptible to it than others is critical for determining how to prevent and treat the disease in at-risk populations. There is currently limited information on how invasive fungal sinusitis spreads, and its relationship with non-invasive forms of the disease is still unknown. However, early research suggests that a compromised immune system and disrupted epithelial integrity are both important risk factors.
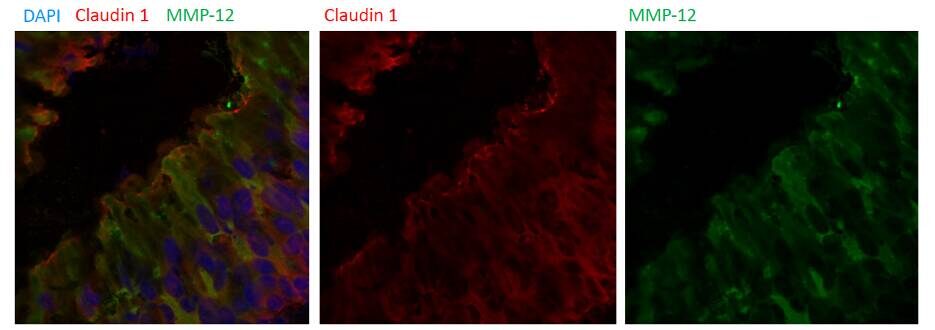
The epithelial barrier is a protective layer of cells in the nose that helps guard the body from harmful substances in the environment. Disrupted epithelial integrity refers to damage or weakness in this barrier. Such weakness may be caused by matrix metalloproteinases (MMPs), enzymes that break down cellular structures in the body. When secreted in response to fungus, MMPs can help control infection by clearing paths for immune cells to reach the infection site. However, if these enzymes damage important protective barriers, it could lead to an unintended fungal invasion.
The long-term goal of this work is to identify specific immune system deficits and alterations in epithelial barrier proteins that are responsible for deficiencies in invasive fungal sinusitis patients. To do this, the research team will use blood and tissue samples to quantify specific MMPs and epithelial integrity proteins in patients with invasive fungal sinusitis and control patients, including those with non-invasive fungal sinusitis. Blood and tissue samples will also be used to identify different types of immune cells associated with survival among invasive fungal sinusitis patients.
Future work will involve developing treatments that target the specific innate immune cell and epithelial deficiencies found in invasive fungal sinusitis patients. Our work to identify specific immune factors associated with invasive fungal sinusitis survival will also allow for targeted treatments in patients who are diagnosed with this disease.
Significance
This work will benefit all immunocompromised patients, especially the bone marrow transplant community, which experiences severe immunosuppression due to medications that are required to deplete the immune system prior to transplant. This highly vulnerable group continues to grow. In 2020, there were 22,013 bone marrow transplants performed, a 61% increase from the rate 5 years prior. It is estimated that the bone marrow transplant population will exceed 500,000 within the next decade.
Further, although this condition is rare in the overall population, the risk in patients with multiple risk factors is over 4%. Our research will benefit this population by contributing to the development of both prevention and treatment options.
There has been some concern that non-invasive forms of fungal sinusitis are more common or more advanced in individuals with lower socioeconomic status. Additionally, as climate change occurs, patients in unexpected areas of the country may be exposed to higher levels of fungus than in the past. Equity in access to care for quick intervention of potential invasive fungal sinusitis will be critical.
Benefits
Demonstrated benefits are those that have been observed and are verifiable.
Potential benefits are those logically expected with moderate to high confidence.
Clinical & medical benefits
This work will lead to treatment and prevention options for invasive fungal sinusitis. Our preliminary data suggests that specific types of immune cells are needed in the initial response to fungal invasion for survival of this aggressive infection. The cell stimulators and infusions that are currently used in invasive fungal sinusitis patients have not improved survival. Our work may lead to the development of more appropriate and targeted immune cell replacements or stimulators, ultimately improving survival rates. potential.
This work will lead to treatment and prevention options for invasive fungal sinusitis. Our initial studies have identified specific enzymes that may be degrading nasal barriers and allowing for fungal invasion. We hope to develop targeted inhibitors to block the action of these enzymes in at-risk patients. potential.
Community & public health benefits
This work will improve life expectancy and quality of life in the immunocompromised, at-risk population by providing improved prevention and treatment options. potential.
Economic benefits
Current treatments for invasive fungal sinusitis, antifungals and surgery, are both expensive and dangerous. Surgery can injure important structures, including the brain and eyes, and lead to significant bleeding. Antifungal medications can affect multiple organs and require close follow-up with laboratory work. This work has the potential to lead to prevention strategies for invasive fungal sinusitis, thereby potentially lowering medical and treatment costs. potential.
Clinical
We hope that our understanding of innate immune deficits in invasive fungal sinusitis patients will lead to potential preventative options for patients who are immunosuppressed or planning to undergo immunosuppression. Additionally, by immunophenotyping invasive fungal sinusitis survival and comparing the immune systems of invasive fungal sinusitis patients who survive the disease to those who do not, we may be able to improve survival by stimulating, supplementing, or replacing critical immune cell types in invasive fungal sinusitis patients.
Community
Currently, survival after invasive fungal sinusitis diagnosis is very poor, with only about 50% of people alive 6 months after diagnosis. While the diagnosis is rare, even in bone marrow transplant patients, it is considered a very deadly disease. Additionally, the morbidity from our current treatment options is unacceptable. Our work has the potential to improve both morbidity and mortality in immunosuppressed patients by either preventing the disease or leading to less toxic and less invasive treatment options.
Economic
The diagnosis and treatment of suspected invasive fungal sinusitis, including Otolaryngology consultation, nasal endoscopy, sinus surgery, and long-term toxic antifungal medications, is expensive. Prevention and improved, targeted treatments for this disease will be beneficial to many patients and will lead to effective, cost-saving practices.
Lessons Learned
Our demonstrated benefits are pending. To date, 100% of patients with suspected invasive fungal sinusitis who have been approached about participation in our study have consented. The involvement from the immunosuppressed patient community to improve the lives of future patients is critical to our success.
1. D’Souza A, Fretham C, Lee SJ, et al. Current Use of and Trends in Hematopoietic Cell Transplantation in the United States. Biology of Blood and Marrow Transplantation. 2020;26(8):e177-e182. doi:10.1016/j.bbmt.2020.04.013
2. Den Beste KA, Hoddeson EK, Parkos CA, Nusrat A, Wise SK. Epithelial permeability alterations in an in vitro air–liquid interface model of allergic fungal rhinosinusitis. Int Forum Allergy Rhinol. 2013;3(1):19-25. doi:10.1002/alr.21077
3. Munyemana M, Pande A, Kallogjeri D, et al. Invasive fungal sinusitis risk factors among immunosuppressed hematopoietic stem cell transplant recipients. Int Forum Allergy Rhinol. 2023;13(11):2113-2118. doi:10.1002/alr.23200
4. Nighot M, Ganapathy AS, Saha K, et al. Matrix Metalloproteinase MMP-12 Promotes Macrophage Transmigration Across Intestinal Epithelial Tight Junctions and Increases Severity of Experimental Colitis. Journal of Crohn’s and Colitis. 2021;15(10):1751-1765. doi:10.1093/ecco-jcc/jjab064
5. Majhail NS, Tao L, Bredeson C, et al. Prevalence of Hematopoietic Cell Transplant Survivors in the United States. Biology of Blood and Marrow Transplantation. 2013;19(10):1498-1501. doi:10.1016/j.bbmt.2013.07.020

