Translational Science Benefits
Summary
Myelodysplastic Syndrome (MDS) is a group of blood cancers that affect blood cells in the bone marrow. In the US, approximately 20,000 new cases are reported every year.1 Advanced age is the main risk factor for MDS, with most people diagnosed between ages 71 and 76.1 From 2012 to 2018, only 37% of patients with MDS were expected to live more than five years.2 People with MDS are more likely to develop Acute Myeloid Leukemia (AML), which can impact the production of red blood cells.3 Like MDS, about 20,000 new cases of AML are reported yearly, with an average age of diagnosis of 65.3 AML patients have a similar 5-year survival rate of 28%,4 and without treatment, AML can progress quickly.5 Treatment decisions for these two cancers rely on patient-specific genetic information about how aggressive the cancer is. More aggressive cancers require intensive treatment with chemotherapy or stem cell transplants, while less aggressive cancers can be treated with less intensive therapies. Current tests are limited, which can result in delayed or lower quality treatment decisions.
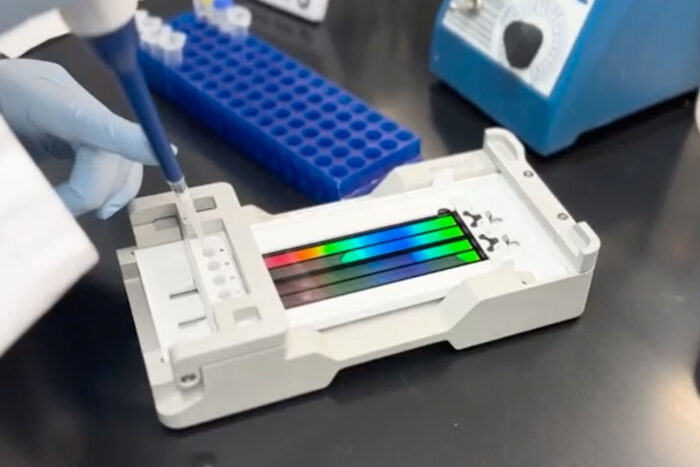
To address this problem, a team of researchers at Washington University created the ChromoSeq test which takes a snapshot of the patient’s genome sequence. Information contained in the snapshot about the order of genetic building blocks helps identify genetic cancer clues that can guide personalized treatment options. Results from ChromoSeq take about seven to ten days.6 Previous tests with the same level of precision took one year, delaying treatment decisions for sick patients. The results from the ChromoSeq testing allow physicians to make timely treatment decisions for their patients.
Significance
With current protocols, physicians piece together the results of three different tests designed to identify genetic changes. They use these results to make treatment decisions for their MDS and AML patients. However, these tests often result in errors. ChromoSeq is revolutionary in that it scans the patient’s entire cancer genome; because it looks at the big picture, it is less prone to error. It can also be adjusted to look for new cancer biomarkers as they are discovered, and it can be modified to look at different types of cancer. Because the ChromoSeq test is reliable and affordable, the Centers for Medicare and Medicaid Services (CMS) have agreed to reimburse the cost of testing. This coverage is significant for many reasons. First, ChromoSeq is the first whole genome sequencing assay to be approved by CMS for cancer. Second, by reimbursing the cost of ChromoSeq, CMS is helping advance health equity. Coverage of ChromoSeq increases healthcare accessibility and improves diagnostic accuracy for Medicaid participants, about half of whom are people of color, and for Medicare participants, most of whom have disabilities or are age 65 or older.7 Finally, CMS’s coverage decision has provided a foundation for future private insurance coverage of ChromoSeq, with potential for increases in healthcare accessibility and quality for those covered by private insurance.
Benefits
Demonstrated benefits are those that have been observed and are verifiable.
Potential benefits are those logically expected with moderate to high confidence.
Developed a new diagnostic test for common blood cancers. demonstrated.
Clinical
ChromoSeq can be adjusted to scan for other cancers, potentially improving diagnostic quality for other cancers. potential.
Clinical
ChromoSeq is a biomedical innovation using whole genome sequencing. demonstrated.
Clinical
The National Comprehensive Cancer Network added whole-genome sequencing (like ChromoSeq) to its AML testing guidelines. demonstrated.
Clinical
Medicare and Medicaid coverage of ChromoSeq increases care access for patients. potential.
Community
Increased accessibility of diagnostic test may increase quality of health care services. potential.
Community
ChromoSeq may lead to improved life expectancy/quality of life for patients. potential.
Community
Medicare and Medicaid coverage of ChromoSeq will reduce costs for care for their enrollees. potential.
Economic
Public insurance coverage of ChromoSeq may lead to private insurance coverage. demonstrated.
Economic
Advancements in genome sequencing technology have reduced testing costs. demonstrated.
Economic
Expanded healthcare access and increased quality may reduce societal burden of disease. potential.
Economic
This research has clinical, community and economic implications. The framework for these implications was derived from the Translational Science Benefits Model created by the Institute of Clinical & Translational Sciences at Washington University in St. Louis.8
Clinical
A collaboration of Washington University in St. Louis researchers resulted in ChromoSeq, a new diagnostic test for the blood cancers AML and MDS. ChromoSeq is superior to previous standard tests for these cancers. It provides rapid and accurate test results which help facilitate timely treatment decisions for patients. The five-year survival rate for both blood cancers combined is less than 33%. ChromoSeq has the potential to improve life expectancy and quality with this enhanced diagnostic information. Because ChromoSeq looks at the entire cancer genome, it is considered unbiased; it can also be adapted to look for additional types of cancer. The success of this technology has prompted the National Comprehensive Cancer Network to add whole-genome sequencing to its AML testing guidelines.9
Community
Because ChromoSeq test results are so conclusive, CMS has agreed to reimburse the cost of testing. With this coverage, physicians across the U.S. who care for Medicare and Medicaid recipients can order ChromoSeq testing. This helps physicians make better treatment decisions for their patients and immediately expands access to care for millions of Americans. With this increased access to care, health care quality should also increase for Medicare and Medicaid participants.
Economic
Medicare and Medicaid’s coverage of ChromoSeq ensures that the patients receiving public insurance have no financial barrier to the test. Private insurance coverage decisions often follow public insurance coverage decisions, so it is reasonable to expect private insurance coverage of tests like ChromoSeq in the future. With increased access to diagnostic testing, appropriate treatments should begin more rapidly, thus potentially reducing societal burden of MDS and AML. Costs associated with longer hospital stays and unnecessary procedures should also be reduced as accurate treatment would start earlier for the patient.
- Myelodysplastic Syndrome (MDS) Research Funded by LLS | Leukemia and Lymphoma Society. Accessed October 18, 2023.
- Blood Cancer Statistics | LLS. Accessed October 18, 2023.
- Vakiti A, Mewawalla P. Acute Myeloid Leukemia. In: StatPearls. StatPearls Publishing; 2023. Accessed October 18, 2023.
- Leukemia – Acute Myeloid – AML – Statistics. Cancer.Net. Published June 25, 2012. Accessed October 18, 2023.
- PDQ Adult Treatment Editorial Board. Adult Acute Lymphoblastic Leukemia Treatment (PDQ®): Health Professional Version. In: PDQ Cancer Information Summaries. National Cancer Institute (US); 2002. Accessed October 18, 2023.
- Duncavage EJ, Schroeder MC, O’Laughlin M, et al. Genome Sequencing as an Alternative to Cytogenetic Analysis in Myeloid Cancers. N Engl J Med. 2021;384(10):924-935.
- Limburg A, Kurczewski A, Udalova V. Enhancing Race and Ethnicity Information in Medicaid Data: The Role of Census Bureau Data.
- Luke DA, Sarli CC, Suiter AM, et al. The Translational Science Benefits Model: a new framework for assessing the health and societal benefits of clinical and translational sciences. Clin Transl Sci. 2018;11(1):77-84.
- National Comprehensive Cancer Network (NCCN). Clinical Practice Guidelines in Oncology (NCCN Guidelines): Acute Myeloid Leukemia. Published online July 11, 2023.
- Bhandari T. Medicare approves WashU Medicine’s whole-genome test for blood cancers. Washington University School of Medicine in St. Louis. Published August 17, 2023.

